To Improve Veteran Care, Outsource Work to Private Sector
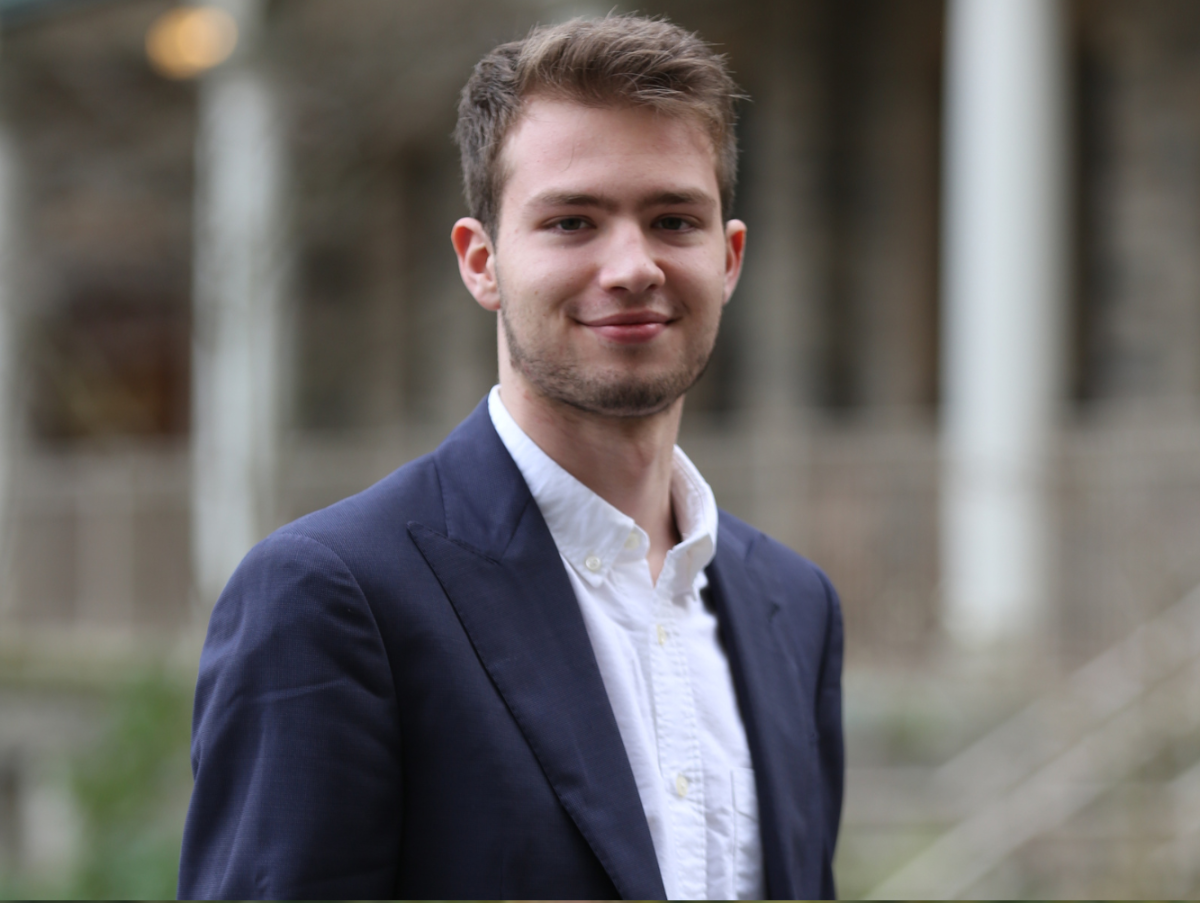
By Dane Salmon
The Veterans Affairs Mission Act was signed into law by President Donald Trump on June 6, 2018. It makes provisions for a $50 billion investment in the Department of Veterans Affairs, or VA, to increase its community care network and help eliminate funding gaps for the VA Choice program. The act helped veterans get healthcare from private sources if they were precluded from using VA resources by distance or if VA wait times were too long. It also gives funds for training VA staff, a review of VA facilities, recruitment of more staff and the seven entities helping veterans get private healthcare into a single program.
This seems to be a move by the administration to help the VA not only modernize its current facilities, but also assist veterans who would be and are left behind by an inefficient and aging network of VA facilities and administration.
Decentralizing parts of the VA network will help fulfill its mission to provide high quality and readily available healthcare to those who fought for our country.
The purpose of the organization is not to control veterans’ healthcare but to help them get it. Those who provide the care are not nearly as important as availability and quality.
The VA’s current resources are hardly able to fill the increasing demand for healthcare for veterans because it is a jack of all trades and a master of none. Helping the VA find the best solutions for veterans should be the purpose of the department’s existence, and decentralization and outsourcing can only help that.
But why can this not be done simply by increasing its funding? Because centralization and government control are inextricably tied with inefficiency. Sacrificing quality and availability of care for centralized control is the worst choice that could be made in the interest of healthcare for veterans, and the very telos of the Department of Veterans Affairs.
Who would stand in the way of better healthcare for veterans for an ill-conceived, micromanag notion of government control of healthcare?
Aside from this reason, we may look to a more concrete one. The VA’s budget last year was $188.65 billion, up from $42.38 billion twenty years ago; an increase of $146.27 billion. They have increased the number of medical facilities by 130 since 2000, now numbering 1,240.
The VA now employs 385,223; this is nearly a 60 percent increase, putting the number of employees at 385,223 as of March 2018.
With the provisions outlined in the Veterans Affairs Mission Act, all of these numbers are likely to grow. However, they still cannot provide adequate healthcare to those to whom the department exists to provide it for.
Now, the idea that this is a move towards privatization is either a misnomer or a false narrative because, as can be seen from the evidence above and the provisions of the recent act, the VA has increased in size since the beginning of this apparent privatization push.
Decentralization and outsourcing is not privatizing, as the act seems to make no mention of private funding of the Department of Veterans Affairs. Government funding of privately-provided healthcare is not privatization. The debate concerning the merits of increased privatization is for a different article.
For now, the situation is that the VA is outsourcing and improving its own facilities to better provide much-needed healthcare for America’s veterans. In the context of the public opinion shift towards Medicare for all, which a recent poll claims 70 percent of Americans support, I hope this will be a slap in the face for the idea.
If we see that private organizations provide better care, almost certainly for a lower cost than inefficient government-administrated and administered healthcare, I hope and expect people will begin to see that government interference almost never makes things better.
If decentralization of healthcare resources and freedom of choice can help veterans, it can certainly help everyone else, lest we fall blindly into the pit of state-run healthcare like Britain’s National Health Service, in which endless legions of bureaucrats decide who can be treated and when, and under which the average person has to wait 18 weeks to see a general practitioner.
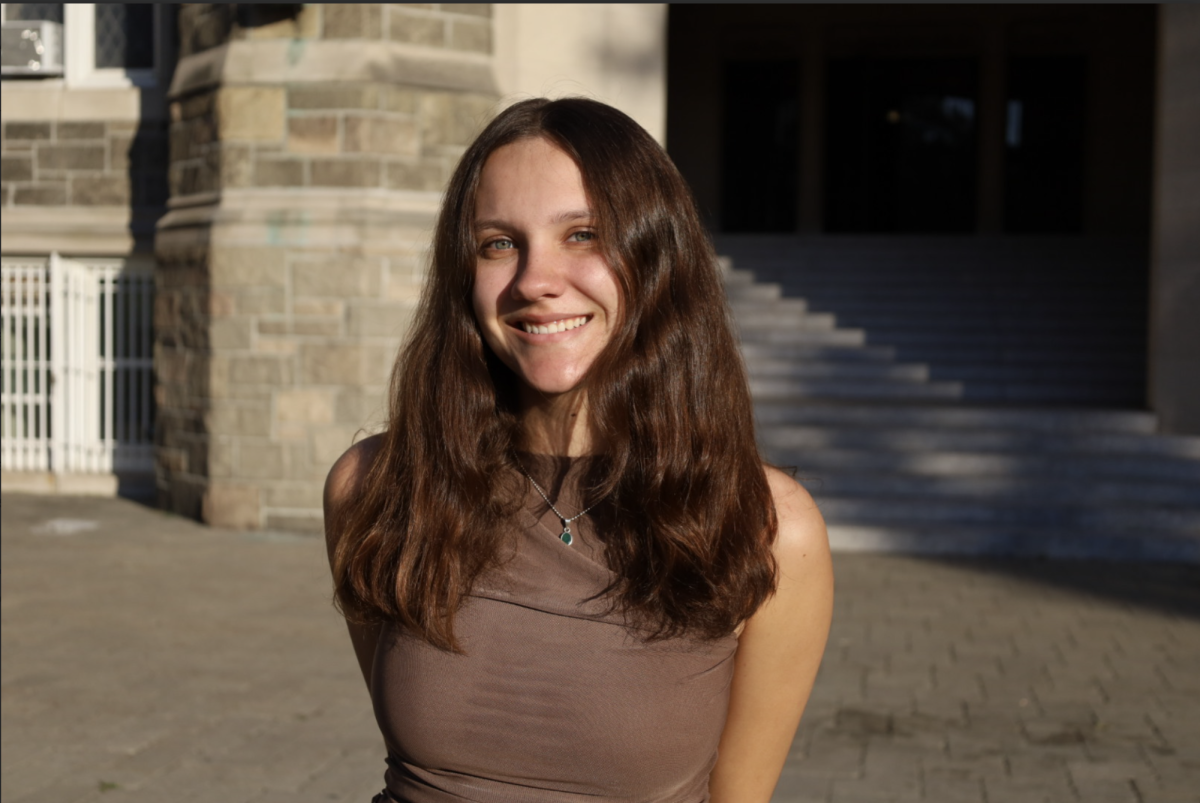
Dane Salmon, FCRH ’21, is a philosophy and economics major from Coppell, Texas.