DEA’s New Regulations Will Hurt Patients
In late February, the Drug Enforcement Administration (DEA) announced that it would be posing restrictions on some of the flexible telehealth policies which were introduced during the COVID-19 pandemic that allowed patients to get their prescription drugs without having to visit doctors in-person, with the public having had until March 31 to comment on these new regulations. These regulations wouldn’t affect telemedicine consultations where controlled medications aren’t being prescribed, telemedicine consultations where the medical practitioner has conducted an in-person examination of the patient before and telemedicine consultations and prescriptions where a patient referred to a medical practitioner has had a chance to do an in-person examination. Instead, they affect telemedicine consultations where a medical practitioner has never conducted an in-person examination of the patient and the patient is prescribed controlled medication. In these cases, the patient would be able to be prescribed a 30 day supply of “Schedule III-V non-narcotic controlled medications” or “buprenorphine for the treatment of opioid use disorder” without an in-person evaluation. However, many say that the new drug policies are a way for the DEA to control the drug supply to counter a severe drug shortage which could be dangerous for patients.
Information on the role of the DEA and pharmaceutical companies is murky and needs to be examined more thoroughly. Every year, the DEA sets up a quota, “a limit on the amount of raw materials for many controlled substances,” that is divided up between manufacturers who can request an increase in their quota which the government either accepts or denies; if the government denies the request, “the Attorney General is supposed to provide a written denial, which the Secretary of the Department of Health and Human Services is supposed to post on the FDA website.” The specific quota each manufacturer gets, how much of their quota manufacturers use and confirmed quota increases are still key information which is unknown. In addition to unknown information, in the U.S., “nearly 80% of the manufacturing facilities that produce these active pharmaceutical ingredients” come from outside the country and it is difficult to keep track of all the manufacturers.
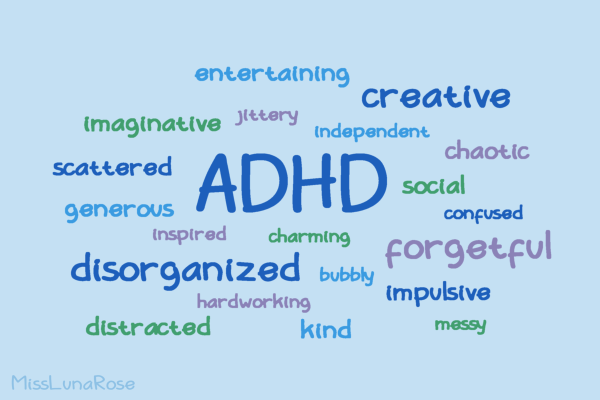
Information on product and manufacturer site quality is also confidential to buyers of these medications, making it difficult to measure the reliability of different manufacturers and understand where ingredients for medications are produced. Manufacturers also don’t need to “publicly explain the reason for their shortages,” further leaving the issues causing these shortages unknown and leaving the U.S. healthcare system in the dark. The U.S. drug shortage isn’t anything new and people have noticed it since the pandemic. The shortage includes a wide variety of drugs from common medications like Adderall to antibiotics like Amoxicillin and drugs used to treat cancer or breathing problems. Unlike other items, it can be challenging to find alternatives for these drugs which leads medical practitioners to make difficult decisions.
The shortage of drugs directly affects patients’ lives where studies find “that people often have worse health outcomes when they can’t be treated with the appropriate medication and even, in some cases, when alternative drugs are used.” In these drug shortages, medical practitioners also have to consider horrible choices in deciding which patients get medication. Lack of information from manufacturers on when they could go bankrupt and shut down leaves hospitals scrambling on how to manage drug shortages. While some hospitals have more resources to deal with drug shortages, many others don’t and not every patient would have access to a hospital with more resources.
Reduced access to drugs would also have more consequences on patients and can lead many to more addiction or to use illegal drugs to self-medicate. This can have devastating effects on patients and their loved ones as they can worsen their illnesses by going down an unclear path. In conclusion, the new DEA policy points to an ineffective way to deal with the medication shortage in America which affects all levels from the overall health system to medical practitioners and patients. There should be more transparency available to drug buyers and the health system on manufacturers and their product quality as well as more investigation drug shortages for manufacturers and how the government can aid in this process.
Saisha Islam, FCRH ’25, is a biology major from New York, N.Y.

Saisha Islam is a senior from the Bronx, N.Y., who is majoring in biological sciences and minoring in English. She first joined The Fordham Ram as a contributing...