Psychiatry Must Have a Strong Social Context
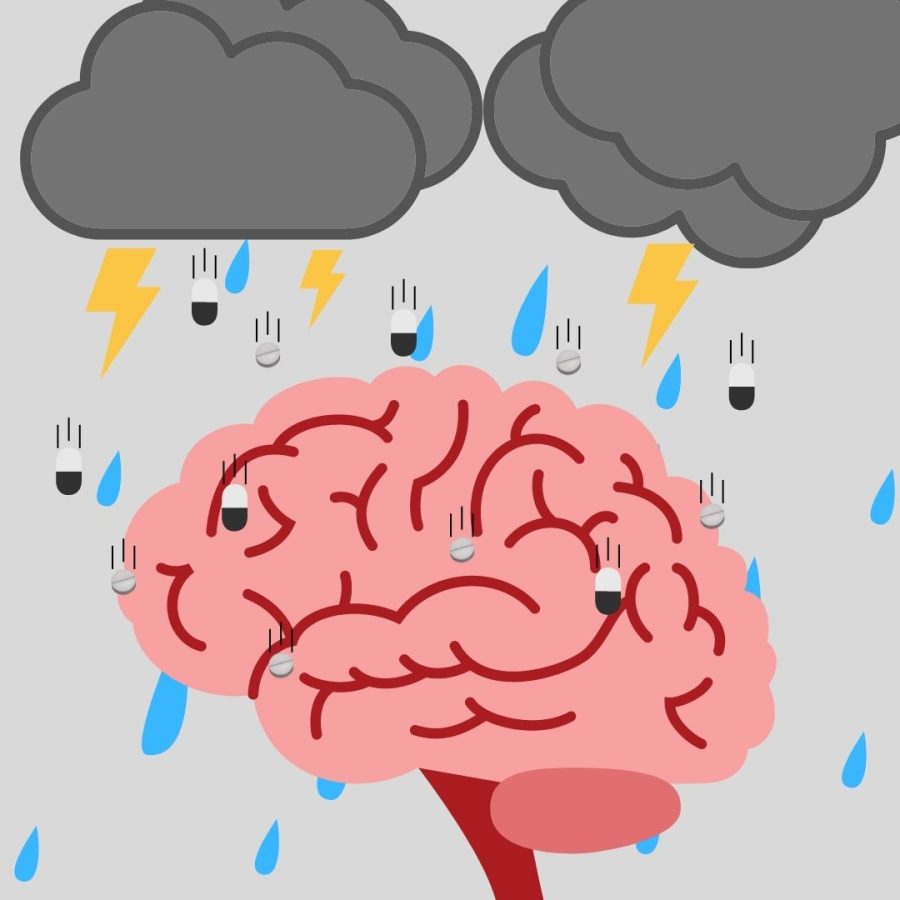
The rise in psychiatric drug prescriptions reveals the need to shift away from corporate biopsychiatry toward social psychiatry. Discourse around mental health in America has been marred by an overemphasis on genetic causes and chemical solutions. This issue likely originates from the interests of pharmaceutical corporations, but has seeped into the moral language of our society.
There is a popular insistence to “just go to therapy” and “take your meds” in America that is truly negligent. This is not to say that medication and therapy are wrong. Many of those who can afford medical treatment clearly benefit from these prescription drugs. Making medication affordable should be a top priority.
However, the most common mental illnesses like depression cannot accurately be understood as a spontaneous neurochemical imbalance, as explained by Noam Shpancer, a professor of psychology and clinical psychologist. At least, there is not enough evidence to definitively link all cases of depression with chemical imbalances. Mental illnesses like depression can be categorized under a biopsychosocial model: negative mental phenomena that emerge on the level of the individual due to the disorganization of our social structures, or a way of considering mind, body and social factors in diagnosing mental illness.
Unfortunately, economic inequality is not going away anytime soon. In the meantime, we need to use modes of psychiatric help that utilize the mind, body and social sciences to address the socioeconomic dimensions of mental illness.
I believe the dominant popular psychiatric discourse has two poles: denial and nihilism. On one end, mental illness is treated as unreal by some people. Chronic issues like depression are denied as the consequences of solely personal choices; some myths include saying that depression can be fixed by eating leafy greens, smiling more and going on a jog. On the other end, some categorize mental illness as hyperreal. It is as if illness is coded into genetic code from birth; it is a fixed part of your identity, something that will forever alienate you from the rest of society. Nothing you do could significantly change it, only mitigate its effects. When this viewpoint is taken, medication is seen as an unambiguous cure. While these might seem like opposite positions, in practice, they lead to similar results. Both encourage individual apathy towards mental health care.
We have to address how young people are coping with these common societal viewpoints, especially since young people are receiving more prescriptions than ever. Younger generations have been more open to the importance of mental health awareness, but still some people fall within the binary of generalized praise of medication and mental illness nihilism. I think this arises from a misunderstanding of genetics.
In most cases, genetic code does not cause mental illness on its own. Instead, it predisposes an individual toward one condition or another given certain environmental conditions. For example, some genetic sequences make people more likely to have depression, but only if they go through significant childhood trauma. Extraordinarily little is written in stone about anyone from birth.
The modern world is built upon pistons, crutches, code, wheelchairs, glasses and medications that augment our bodily capabilities to increase our autonomy and welfare. Yet, when it comes to our mental health, I think some young people simply submit to it, ingrain it into their identity, think of themselves as wholly “depressed” or “anxious” people. Their sense of how tough it is to fix these issues is genuine and entirely justified. However, lots of mental health issues do not originate from just the individual, but also the societal fabric they are raised within.
Some young people submit to the concept of mental illness as an unchangeable individual identity, but this frustration should be directed toward the social structures that trigger these conditions.
This is not solely a juvenile position. Contemporary politics often encourages a sense of social nihilism. Consider the 2008 financial crash, the 2016 election and the COVID-19 pandemic. These events feel as if they are no one’s decision, like they simply occurred. Society tries as hard as possible to return to baseline. Banks are bailed out. Mask mandates are lifted preemptively. The “new normal” is announced. In short, many Americans live in passive times. Since social factors play a large role in mental disorders and many Americans lack social agency, it is exactly this political nihilism that makes many feel hopeless and alone with their mental health issues. These political events explain why some may abandon the role of social factors on mental health and instead assign the blame to something fundamental about themselves, even if that goes against the science.
The real issue is not that there are too many prescribed medications, but that we are ignoring the social pandemics that spread alongside the biological. We cannot resolve these issues only through individual medication and therapy. We need to revise the model of individualistic neurochemical psychiatry in favor of holistic psychiatry that is focused on the mind, body and social factors.
Alexander Gannon, FCRH ’25, is a neuroscience major from Allentown, P.A.